Oral surgery refers to any surgical procedure performed on the teeth, gums, jaw, or related structures. These procedures are designed to treat dental issues that cannot be resolved with traditional, non-surgical methods. While many of these treatments are routine and common in dental care, oral surgery is typically necessary when the condition of the teeth or mouth requires more advanced intervention for optimal results.
Our team is trained to perform a variety of oral surgeries, ensuring that you receive safe, effective treatment tailored to your unique needs.
A tooth extraction is the removal of a tooth from its socket in the bone. While many teeth can be extracted relatively easily, some may require a more advanced surgical approach, especially if the tooth is broken, impacted, or below the gumline. A single tooth extraction may be necessary for reasons such as:
A simple extraction is typically performed when the tooth is fully visible above the gumline. This type of extraction can usually be done in a dental office under local anesthesia. The dentist will loosen the tooth with special instruments and remove it without the need for incisions or any bone removal.
In more complex cases, a surgical extraction may be required. This is typically the case if the tooth is broken below the gumline, impacted, or has not fully erupted. A surgical extraction involves making a small incision in the gum tissue to access the tooth. Sometimes, the tooth may need to be sectioned into smaller pieces or some bone may need to be removed for easier removal. Surgical extractions are usually performed under local anesthesia with or without sedation, depending on the complexity of the procedure and the patient’s comfort level.
A condition where the blood clot at the extraction site becomes dislodged, causing pain and slowing healing. We’ll provide instructions to help avoid this.
Although rare, an infection can occur at the extraction site. If you notice increased swelling, pus, or fever, contact us immediately.
Please contact us if you experience any of the following after the extraction:
After your procedure, you will have gauze placed in your mouth to help control bleeding. Keep the gauze in place with gentle pressure for 30 minutes. After that, you may remove it if bleeding has slowed down. If bleeding continues, replace the gauze and repeat the pressure for another 30 minutes.
You may experience some soreness after the anesthesia wears off. Over-the-counter pain relievers or any prescribed medication will help manage this discomfort. We recommend 600mg Ibuprofen every six hours until pain subsides. If the pain is not alleviated, you may try combining 500mg Tylenol with the Ibuprofen, but in an alternating sequence- ie. Ibuprofen- then Tylenol three hours after that, then your next Ibuprofen three hours after that and so forth.
You can begin eating a soft, cold meal right after your procedure. Continue on a soft food diet for the next 5 days. Foods such as yogurt, applesauce, smoothies, and mashed potatoes are great choices. Avoid hard, crunchy, or hot foods that can irritate the surgical sites. Drink plenty of fluids to stay hydrated, but avoid using a straw, as the suction can disrupt the healing process and increase the risk of dry socket.
For the first 5 days after surgery, avoid the following:
• Swishing or spitting forcefully
• Eating or drinking hot foods or beverages
• Drinking through a straw
• Consuming carbonated drinks or alcohol
• Lifting heavy objects (more than 15 pounds)
• Engaging in strenuous physical activities or exercise
Gently brush your teeth, avoiding the extraction site, until the area heals. Gently rinse with warm salt water starting 24 hours after the procedure to help reduce the risk of infection.
Apply ice pack to your jaw for 15 minutes at a time, especially during the first 48 hours. Ice will help minimize bruising and swelling.
At Intermountain Dental, we prioritize your long-term oral health, and that includes addressing issues related to wisdom teeth. Wisdom teeth can lead to a variety of complications due to their late eruption. Read on to learn more about the potential problems caused by wisdom teeth and why removal may be the best option.
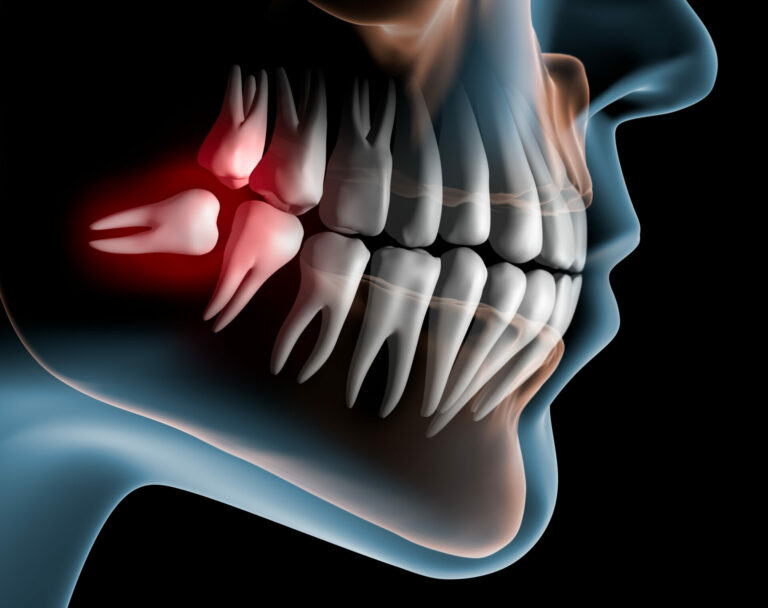
Wisdom teeth often cause challenges because they typically emerge in late adolescence or early adulthood, a time when the mouth may not have sufficient space for them. Common issues associated with wisdom teeth include:
As wisdom teeth attempt to emerge, they may push against surrounding teeth, leading to overcrowding. This can affect the alignment of your other teeth, making it more difficult to maintain proper oral hygiene and causing discomfort.
When there is not enough space for the wisdom teeth to emerge fully, they may become impacted. This can lead to significant pain, swelling, and even infection. Impacted teeth may also push against adjacent teeth, creating further complications.
Wisdom teeth may come in at awkward angles, leading to bite problems and misalignment. This can affect how your teeth come together when you chew, resulting in discomfort or difficulty with proper biting and chewing.
If a wisdom tooth only partially erupts, it can create pockets around the tooth where bacteria can accumulate. This can increase the risk of gum disease, infections, and discomfort due to inflammation.
In some cases, the development of cysts or tumors in the jawbone can be triggered by wisdom teeth. While rare, these growths can cause serious damage to the surrounding bone and tissue.
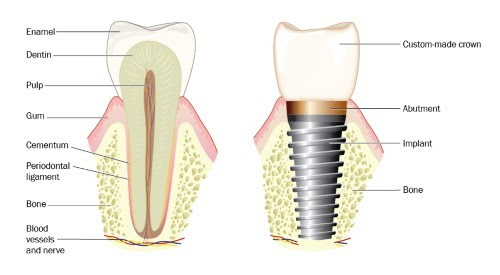
Dental implants are one of the biggest and most successful advances in modern dentistry. They are an effective, long-term option if you have missing teeth or wear dentures that are uncomfortable. An implant is a small, titanium root-shaped screw that is inserted into the jawbone to replace a missing tooth or to help retain dentures. The implant fuses with the bone and healing is usually completed within 3-4 months. This provides a solid foundation for an abutment and dental crown. The implant looks, feels and acts like a real tooth, and if properly cared for, can last a lifetime.
There are several advantages to choosing dental implants over other options such as dental bridges or partial dentures. Some of these benefits may include:
There are very few conditions that contraindicate the placement of dental implants. An ideal candidate is in good general and oral health and has adequate jawbone and healthy gum tissue to support the implant. Although few, there are some conditions that could impact the success of an implant, such as:

Dental Implants have become the treatment of choice for missing teeth. The loss of all of your teeth brings a variety of complications that can have a severe impact on your physical and emotional health. Traditional dentures have limited success, as they are not stable and secured. Dentures can make it difficult to speak clearly and to effectively chew the foods you desire. Discomfort and soreness, muscular issues and headaches almost always accompany dentures as they slide and shift around as you move your mouth. Implant retained dentures are an innovative restoration that provides denture wearers the quality of life and oral health they so much desire. Special attachments on the implants help secure the denture in place, thus eliminating all of the problems associated with the movement of the denture. Implant retained dentures are life changing.
The procedure involves the careful removal of excess gum tissue and sometimes a small amount of bone to expose more of the tooth’s surface. Local anesthesia is used to ensure your comfort throughout the process.
Typically takes 1-2 hours.
Most patients experience mild discomfort for a few days, which can be managed with over-the-counter pain relief. Swelling is common, but should subside within a week.
Follow-up visits will ensure proper healing, and our team will guide you through aftercare instructions for optimal results.
Typically takes around 15-30 minutes.
Most patients experience minimal discomfort following the procedure. The recovery time is usually short, with many patients able to resume normal activities within a few days.
We will provide detailed aftercare instructions to promote healing and reduce the risk of complications.
A frenectomy is commonly recommended for: