Temporomandibular Joint (TMJ) Disorders
What is TMJ disorder?
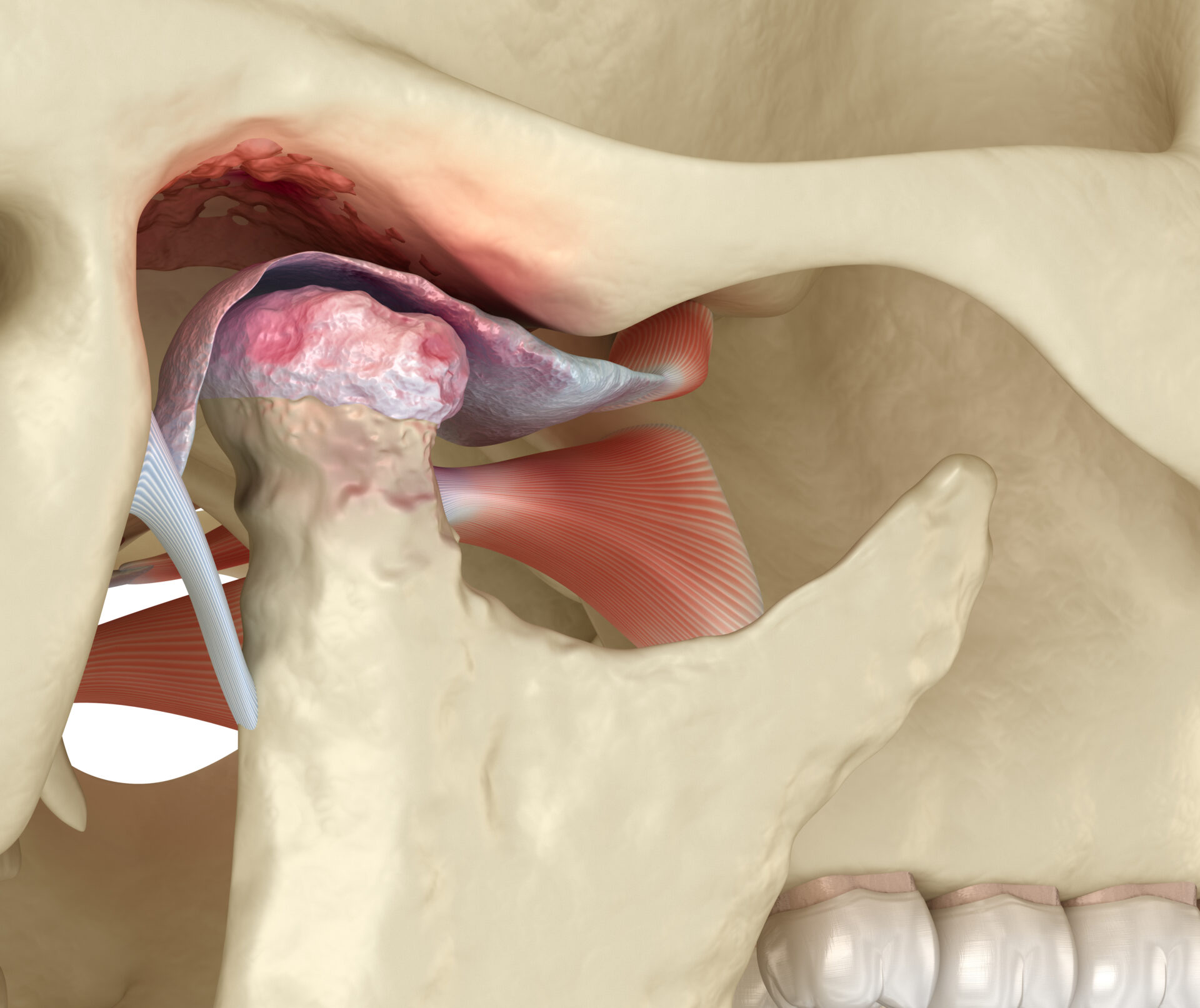
The temporomandibular joint (TMJ) connects the lower jaw (mandible) to the skull and allows for movement like opening and closing the mouth, chewing, and speaking. TMJ disorder occur when the joint or muscles around it are injured, overworked, or misaligned, leading to pain and dysfunction. You might hear people call these conditions TMJ. But “TMJ” refers to your actual jaw joint, while “TMD” stands for temporomandibular joint disfunction, or disorder. There’s no singular cause of TMD. Rather, it can be a result of many different factors or a combination of factors.
Common Causes
- Injury or Trauma — A blow to the jaw or head can damage the TMJ.
- Teeth Grinding (Buxism) — Frequent grinding or clenching of teeth, espeicially during sleep, can strain the TMJ. This tends to be one of the most common causes of TMJ disorder.
- Arthritis — Osteoarthritis or rheumatoid arthritis can affect the TMJ.
- Jaw Misalignment (Malocclusion) – If your bite is not aligned properly, it can put extra stress on the joint.
- Stress – Increased stress can lead to muscle tension in the jaw and facial muscles, aggravating TMJ issues.
Common Symptoms
- Jaw Pain or Tenderness to palpation
- Clicking or Popping Sounds when moving the jaw
- Limited Jaw Movement (difficulty opening or closing the mouth)
- Headaches and Migraines
- Earaches (without ear infections)
- Neck and Shoulder Pain
- Facial Pain or Muscle Stiffness
How is TMJ Diagnosed?
- Physical Examination — A dentist or doctor will check for tenderness, swelling, or clicking noises in the jaw.
- X-Rays and Imaging — To check for structural issues, such as arthritis or joint damage.
- MRI or CT Scans — In some cases, these can be used to examine soft tissue and bone in more detail.
Conservative Treatment Options
Lifestyle Changes
- Stress management: Relaxation techniques to reduce jaw clenching.
- Dietary Changes: Soft foods and avoiding hard, chewy foods.
Physical Therapy
- Stretching and strengthening exercises for jaw muscles.
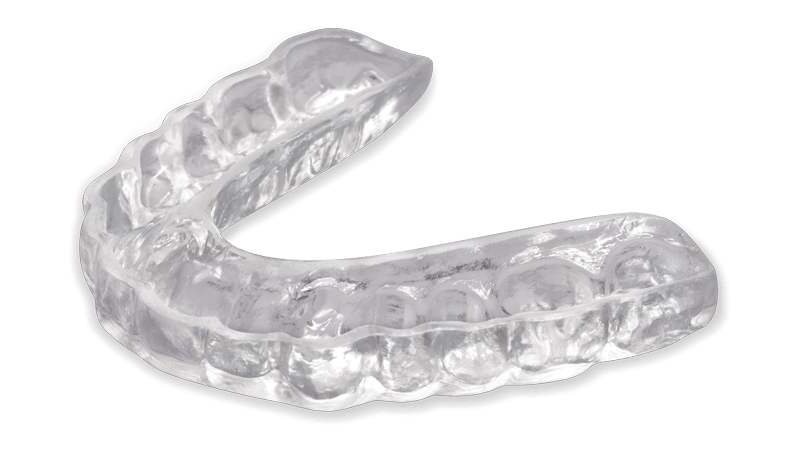
Mouthguards and Splints
- Custom-made to prevent teeth grinding and to stabilize the jaw.
Medications
- Pain relievers, muscle relaxants, and anti-inflammatory drugs.
Heat and Ice Therapy
- Alternating heat and cold can reduce inflammation and alleviate pain.
Advanced Treatment Options (if necessary):
- Injections: Corticosteroid or botulinum toxin (Botox) injections to reduce pain.
- Surgical Options: In rare cases, surgery may be required for severe TMJ disorders.
Prevention Tips
Avoid Chewing Gum: Repeated chewing can strain the jaw muscles.
Manage Stress: Practice relaxation techniques such as meditation or yoga.
Maintain Proper Posture: Poor posture can affect your jaw alignment.
Visit Your Dentist Regularly: Routine chekcups to catch early signs of TMJ issues.
FAQs about TMJ Disorders
How long does it take to recover from TMJ disorder?
Recovery time depends on the severity of the condition. Mild cases can improve within a few weeks, while more severe cases may require longer treatment.
Can TMJ cause ear pain?
Yes, TMJ disorders often cause symptoms similar to ear infections, including earaches or a feeling of fullness in the ear.
Is surgery the only option if TMJ pain doesn't go away?
No, surgery is typically considered a last resort after other treatments have been tried.
Need Help with TMJ Pain?
If you are experiencing symptoms of TMJ disorder, Dr. Duke and his staff can help diagnose and create a personalized treatment plan. We’re here to help you regain comfort and improve your quality of life.
